Ninety two percent of consumers who met with in-person assisters (IPAs) were able to get the information they needed about enrolling in health coverage during open enrollment last year, according to a new study. However, those seeking to enroll in health coverage did face some barriers. These successes and setbacks highlight the need for more outreach and information about health coverage eligibility for Arkansans. Unfortunately, the Legislature voted last year to restrict outreach and education efforts around the Affordable Care Act and Arkansas’s own Private Option entirely.
The new report, “Getting In: Improving Consumer-Friendly Enrollment in Arkansas,” was released by Arkansas Advocates for Children and Families (AACF). It provides recommendations for improving the consumer experience going forward, and offers insight for open enrollment in 2015. The report explains the importance of outreach and in-person assistance for helping consumers enroll in affordable health coverage.
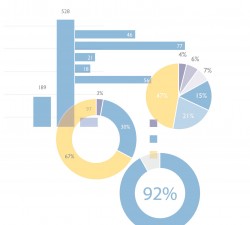
AACF worked with three in-person assisters sites across Arkansas to collect data reported voluntarily by consumers and assisters to inform improvements to the consumer experience. AACF collected 823 consumer surveys and held a focus group with assisters to get their thoughts on the enrollment process. The results show that the vast majority (92 percent) of consumers who met with in-person assisters were able to get the information they needed about health coverage eligibility. However, barriers to full enrollment were as follows:
- Technological issues were the biggest barrier to completing enrollment, including system freezes, data transfers betweenHealthcare.gov and the state system, or having to return at a later date to complete Private Option plan selection.
- Families in complex situations, immigrants, or those with little credit history had more trouble completing an enrollment through one visit.
IPAs suggested improvements for enrollment including training and technical assistance, identity verification, and best practices for consumers going into open enrollment 2015. Data collected for this report show that an improved consumer experience is possible if Arkansas and the federal Marketplace take the following steps:
- Continue funding in-person assistance and public education in coming years.
- Streamline “no wrong door” enrollment process – both on the consumer-facing side and behind the scenes.
- Train assisters on Access. Arkansas.gov and details about the Private Option, Medicaid, and ARKids First.
- Improve the identity verification process.
- Add needed staff at DHS to handle technical issues and support.
- Develop appropriate renewal and cancellation procedures.
For more details on consumer-friendly enrollment, please see the attached report.
