Considering Arkansas is one of the 10 poorest states in the nation, with a poverty rate of 16.3% and a child poverty rate of 22%, it should come as no surprise that a large number of Arkansans need health care coverage through Medicaid. But thousands of Arkansans, including children, have lost their Medicaid coverage in the past month, despite being eligible for the program based on their income.
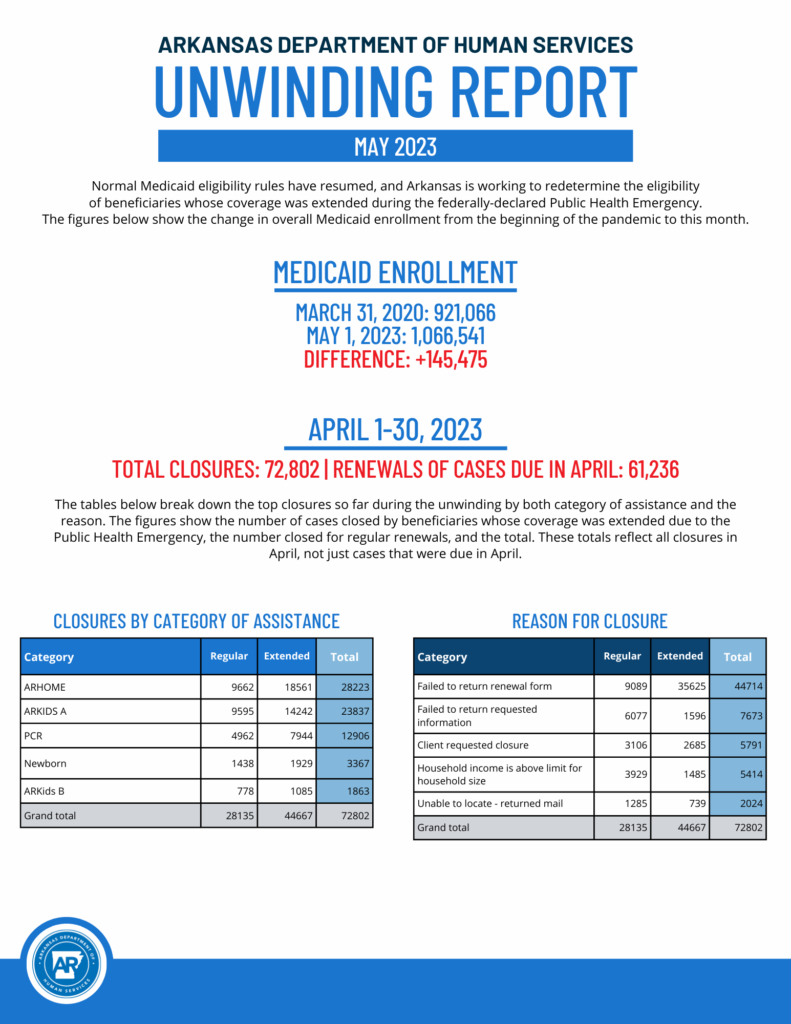
A report released on May 8, 2023, by Arkansans DHS shows 72,802 Arkansans lost their Medicaid coverage, including 44,667 as a result of COVID related Medicaid policy.
Why is this happening? Because the Arkansas Legislature decided in 2021 that Arkansas would conduct the “Medicaid unwinding” in just six months. The Centers for Medicare and Medicaid Services warned that moving so quickly would increase the risk of terminating a lot of people who are in fact eligible. But Arkansas leaders have been determined to “save” the state money by kicking people off Medicaid, putting our state in this unconscionable situation.
What can be done? Arkansas should pause procedural terminations until they figure out why so many people are losing coverage without a true determination of being ineligible based on income.
A bit of background
Access to health care is too often talked about like it’s a luxury, when it is a necessity for a healthy, productive population. People who are unable to keep up their health without regular medical care are less likely to become or stay employed.
The COVID-19 pandemic and the economic downturn that followed negatively affected the finances of many Arkansas workers and families. Many lost their jobs, their paychecks and, in many cases, their health care coverage. As a result, many became eligible for Medicaid coverage.
Because of the public health emergency, the federal government put Medicaid rule changes in place in March 2020 to protect health care coverage for struggling families. The rule changes kept Medicaid coverage in place throughout the pandemic for those already approved, as well as for those who obtained coverage during the pandemic. Medicaid coverage was maintained for all cases except for deaths, requests for Medicaid coverage to end, incarceration, and moving out of state. Between March 31, 2020, and May 1, 2023, Arkansas’s Medicaid enrollment increased from 921,066 to 1,066,541, an increase of over 145,000.
The Arkansas Department of Human Services (DHS) began sending out notices in February for people to renew their enrollment in Medicaid, and as of April 1, Medicaid was allowed to terminate coverage for people who were no longer eligible or who did not verify eligibility according to pre-COVID eligibility rules.
ARHOME, ARKids, and Parent Caretaker are the top three categories of Medicaid service included in the first group to receive notices for renewals/terminations of their Medicaid coverage. These groups include more than 300,000 people identified by DHS who started losing their Medicaid in April.
Our worry at Arkansas Advocates for Children and Families has been that families and individuals will fall through the cracks and lose their health care coverage, despite the outreach efforts of Arkansas DHS. Unfortunately, these concerns have been borne out by this first report.
We are right to be concerned
In this first month, 29,067 children lost coverage in the ARKids A, ARKids B, and Newborn categories. In addition to these children, almost 13,000 Parents and Caretaker Relatives also lost their coverage. Another 28,223 adults in the ARHOME Medicaid Expansion category lost coverage. The report does not show how many of the children and adults are in the same households. Of the total cases closed, only 5,414 were closed based on families being ineligible due to income, while 5,791 were closed per client request. Those families who are over income should be immediately referred to the Health Information Marketplace where they may be eligible to obtain coverage.
We are most concerned about people losing health care access unnecessarily. About 82% of the total cases closed (54,411 out of 65,616) were closed because of bureaucratic or paperwork issues and not because of a true determination of ineligibility. The report shows 44,714 failed to return renewal forms, 7,673 failed to return other requested information, and 2,024 were unable to be located.
Over the last three years, people struggling to maintain housing and other basic needs may have moved several times or may be unhoused at this time thus they may lack a stable address or other contact information. Therefore, greater efforts need to be made for outreach to homeless programs, and shelters for youth. Others may be unreachable due to changes in medical status. Medicaid disenrollment will not only affect primary care providers such as doctor’s offices and clinics, many school children will have their therapy services disrupted that are received through school-based clinics. Those seeking coverage as new applicants will have their approvals delayed because of the sheer volume of cases being processed by the eligibility workers. We are extremely concerned for the reasons stated above.