If you missed the blogs on managed care and private option changes, check those out before reading this final blog in our series on health care reform. Today, we will look at work requirements in Medicaid.
After months of meetings to determine the future of the health care system in Arkansas, the Health Reform Legislative Task Force will release recommendations this week. Work requirements are at the core of health reform options the Governor has endorsed. At AACF, we think work requirements for health coverage undermine the purpose of Medicaid, which is to make coverage affordable to low income families.
Variations of a work requirement have been included in Medicaid expansion plans in other states, especially in states trying to create a plan more appealing to conservative lawmakers. The Arkansas proposal would make a referral for a work-training program part of the enrollment process.
The recommendation ties ongoing eligibility to meeting work-training requirements. If the enrollee does not participate in training, they will be subject to a premium and will be locked out of covering for missing payments. So far, no state has received approval to tie any type of mandatory work requirements to eligibility. Pennsylvania proposed a voluntary work search program, after unsuccessfully attempting to make work a condition of Medicaid eligibility.
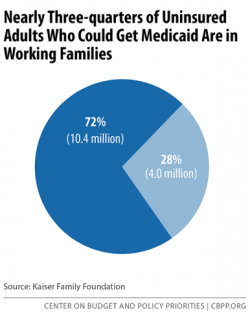
In fact, work requirements are not necessary. Research shows about 75 percent of uninsured adults live in a family with at least one full or part-time worker. Over half of enrollees actually work full or part-time. Private Option can assist with employment by helping people stay healthy enough to work. For individuals not working, the reasons include caring for a family member, looking for work, attending school, or being ill or disabled.
The Private Option also removes work disincentives among low-income parents. Before expansion, parents with very low incomes enrolled in Medicaid risked losing their health coverage if they increased their salary or worked more hours.
For example, a parent in a family of four qualified for Medicaid in Arkansas if they earned less than $4,123 (based on 17% of the federal poverty level in 2015). With the Private Option, if that same family’s income increased to $33,465, a working parent would be able to maintain their coverage and make an affordable, monthly contribution. If they took an even higher paying job, the parent may qualify for assistance (through a tax credit) paying their premium on a Marketplace plan.
