
Read Part 1 and Part 2 of this blog series.
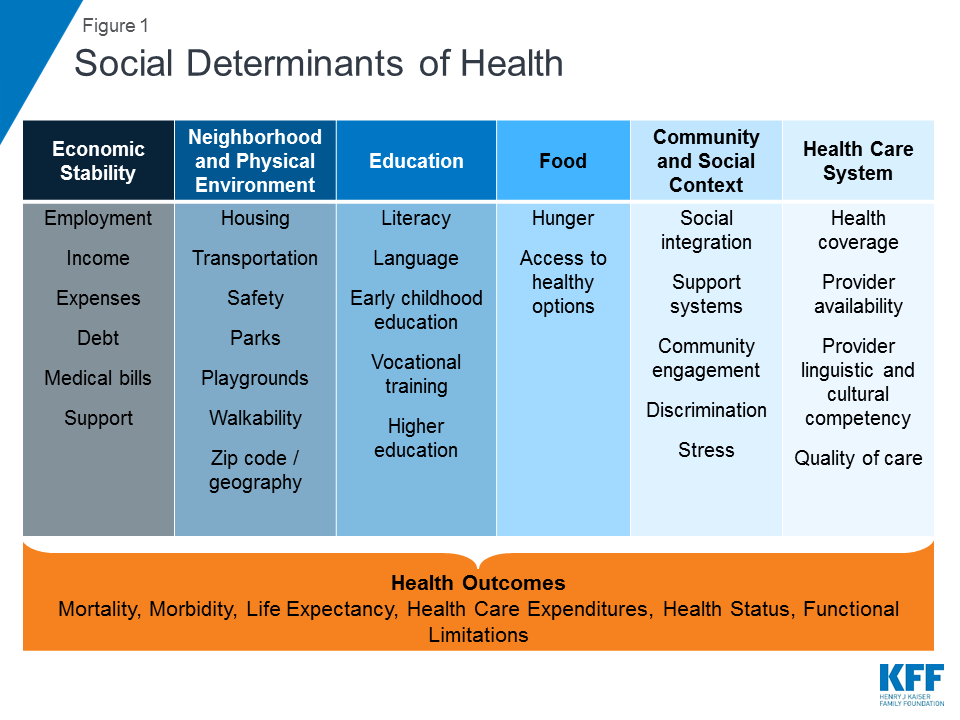
In the final installment for the blog series “Creating a Healthier Arkansas for Black Women,” we discuss the non-clinical factors that impact our health and well-being. Social determinants of health are factors that have been shaped by social policies and play a key role in our health in various ways. They are the conditions in the places that people live, learn, work, and play that impact health risks and outcomes. There are six different domains within the social determinants of health: economic stability, neighborhood and physical environment, education, food, community and social context, and the health care system. When these various domains are combined with systemic and institutional racism, they can result in devastating outcomes for Black women’s health.
Economic Stability
A person’s economic stability plays a large role in their ability to be healthy and stay healthy. Black women earn on average $5,500 less per year than the average woman in the United States. In Arkansas, the median annual income for Black women who work full-time year-round was $28,018, compared to White women who made $33,943 in 2016. Black women are 50% more likely than White women to be the primary source of economic support for their families. They also experience higher rates of unemployment and poverty compared to their counterparts.
Neighborhood and Physical Environment
An example of how systemic racism influences health outcomes is the now illegal practice of “redlining,” which started in the 1930s and denied or selectively raised prices (mortgages, loans, etc.) to residents of redlined neighborhoods. Redlined communities were deemed “hazardous” for lending and were predominantly low- and moderate-income Black neighborhoods. These neighborhoods were outlined in red on maps, and the maps were used to deny mortgages, loans, insurance, and other financial services to residents in those areas and to keep neighborhoods segregated. Redlining reinforced the discriminatory distribution of resources and services and is a significant underlying cause of the poor health outcomes in Black communities.
Arkansas was not exempt from the practice of redlining, especially in its urban communities such as Little Rock, which resulted in highly segregated communities. Little Rock is distinctly separated today by race and socioeconomic status. On the east of I-30 and to the south of I-630, the communities are predominantly Black and have been deprived of necessary economic resources, while the communities to the west of I-430 and north of I-630 are predominantly White and have been equipped economically with an excess of resources. The economic investments in White communities have created lasting effects on the quality of educational systems, neighborhood infrastructures, and healthcare systems.
Education
How much people earn affects where they can afford to live, which then can determine the quality of education resources available for their children. In the city of Little Rock, the effects of residential segregation have left the city divided. White families left the south and southwestern parts of Little Rock for other regions of the city. The schools north of Interstate 630 have more White students, resources, and have better state educational assessments. The schools south of the interstate have more Black students, fewer resources, and have had lower scores on these assessments.
Also, the level of educational attainment achieved plays a role in household income and the ability to create financial security and generational wealth. Parents’ wealth shapes their children’s educational, economic, and social opportunities, which can, in turn, shape their children’s health throughout life.
Food
Inequitable access to healthy food options contributes to health disparities. Greater food access exists in predominantly White and gentrifying neighborhoods (gentrifying is the practice of displacing community members from neighborhoods that were historically excluded from receiving financial resources as wealthier individuals buy out housing and businesses and market them to middle- and upper-class individuals). In contrast, low-income communities of color have experienced more fresh food retailers and full-service supermarkets disappearing from their neighborhoods, which in turn creates food deserts (communities that lack access to affordable and healthy food options). Research has shown that Black communities have the fewest supermarkets at all levels of poverty, while White communities have the most.
Community and Social Context
Different community and social factors also impact Black women’s health. For example, stress, marginalization, and discrimination can have devastating effects on an individuals’ overall health. Weathering, a term coined by Dr. Arline Geronimus, states that the “health of African American women may begin to deteriorate in early adulthood as a physical consequence of cumulative socioeconomic disadvantage.”
Health Care System
Poor rural and urban communities experience more limited access to health care. There have been 98 complete closures of rural hospital facilities in the country since 2005, mostly in the South. Medicaid expansion has helped Arkansas avoid the high number of hospital closures that neighboring southern states have experienced. In 2019, Arkansas did experience the closure of De Queen Medical Center in Sevier County. This has resulted in community members having to travel more than 30 miles to receive medical treatment with comparable services and qualifications to the De Queen Medical Center. In addition, the pandemic exposed a major issue with broadband access. Arkansas ranks 50th in connectivity in the country. This impacts the ability for communities to have access to telemedicine services when they live far from facilities that can meet their health care needs.
The social determinants of health combined with the interrelated social and economic systems that individuals must interact with, impact their health. When you add racism to the mix, more inequitable outcomes will emerge and create additional barriers for Black women to overcome in regard to their overall health.
What can be done?
Arkansas can and should implement these policy solutions that will address social determinants of health and improve access to affordable and high-quality health care for Black women throughout the state.
- Create policies with an intentional racial equity lens
- Continue expanding Medicaid benefits, including postpartum coverage
- Integrate health care access into public schools
- Ensure technological accessibility for Black families
- Increase the number of Black professionals in the medical field
- Improve the quality of care for Black women
Policymakers, health care professionals, and communities must work together to improve Black women’s health.
